DPC Report Card on Medigap Coverage for
ESRD Patients Under 65 Years of Age

61% of ESRD patients are under 65 years old, but only 11% currently have Medigap coverage.
We must do better!
Medigap provides dialysis patients with financial security and access to lifesaving transplant surgery. Medicare only pays for 80% of an individual’s health care costs, making access to Medigap coverage critical for helping dialysis patients cover the remaining 20%. We need your support to help ensure all dialysis patients gain access to Medigap coverage regardless of age. Contact your Members of Congress today.
- All States
- Grade: A (8)
- Grade: B (11)
- Grade: C (15)
- Grade: D (14)
- Grade: F (4)
DPC Grades Based on Patient Access & Affordability:
A State requires all/most plans to be offered and affordable to ESRD patients under 65.
B State requires some plans to be offered and affordable to ESRD patients under 65. C State requires some plans to be offered, but they are not affordable to most ESRD patients under 65. D State does not require coverage. Some plans are offered, but they are not affordable to most ESRD patients under 65. F State excludes coverage. Some plans may be offered, but they are not affordable to most ESRD patients under 65.Medigap Coverage
While Original Medicare covers 80% of medical costs for eligible beneficiaries, those without any type of supplemental insurance policy – such as Medigap or employer-sponsored secondary insurance – individuals must pay the remaining 20% co-insurance, co-pays and deductibles on their own. Since original Medicare has no annual cap for the 20% out-of-pocket co-insurance expenses, this can cause serious financial strain for many Medicare beneficiaries. Some End Stage Renal Disease (ESRD) patients under age 65 who lack access to supplemental insurance are forced to spend down their assets to become eligible for Medicaid coverage. This is financially devastating for these individuals and, in the end, will cost the State – and its taxpayers – more money.
Medigap is a supplemental insurance policy option specifically for Medicare beneficiaries designed to fill the “gaps” in Original Medicare coverage to provide greater financial stability and security for patients. Patients with access to Medigap select an available plan option offered by commercial insurers and pay a fixed monthly premium amount that helps cover and cap their out-of-pocket co-pays and deductibles that Medicare alone doesn’t cover. The problem, however, is that Medigap coverage isn’t currently accessible to all ESRD patients who are on Medicare.
When Medigap plans were first introduced, Congress only guaranteed issue of these plans to traditional Medicare beneficiaries (those age 65 and older who are enrolled in Medicare Parts A and B) without consumer protections and did not extend this protection to disability and ESRD patients who obtain Medicare coverage prior to age 65. Without a federal mandate to extend coverage to all Medicare-eligible beneficiaries regardless of age, states are left to determine their own Medigap policy for disability and ESRD patients under age 65. People on dialysis face serious financial struggles and difficulty accessing kidney transplantation in areas where Medigap coverage is not accessible. That’s why DPC continues to advocate for every person on dialysis to be able to purchase affordable and nondiscriminatory Medigap coverage regardless of age.
Health policy experts often criticize Medigap’s relief from cost sharing as adding to Medicare expenditures. However, using Medicare cost data from 2017-2019, HMA estimated that extending Medigap coverage to all ESRD patients under the age of 65 would only add about $50 million in federal expenditures over the next 10 years. HMA actuaries compared the utilization of services by dual eligible dialysis patients vs. Medicare-only dialysis beneficiaries, and found that the one relevant increase in cost was in drug spend. HMA suspects that by expanding access to Medigap coverage, more dialysis patients will have the money to pay for all of their prescribed medications, as their supplemental insurance would now cover their other health care related expenses. Therefore, HMA projected a de minimis cost increase to Medicare due to increased utilization under Part D following the expansion of Medigap access to patients under 65 years of age. At the same time, the potential increase in medication adherence could lead to better health outcomes and reduced complications.
Related Information
Upcoming Open Enrollment Deadlines for Nevada Dialysis Patients
In a major victory for under age 65 Nevadans living on dialysis, Senate Bill 292 became law earlier this year. SB 292 provides access for under-age 65 dialysis patients to purchase affordable Medigap insurance [...]
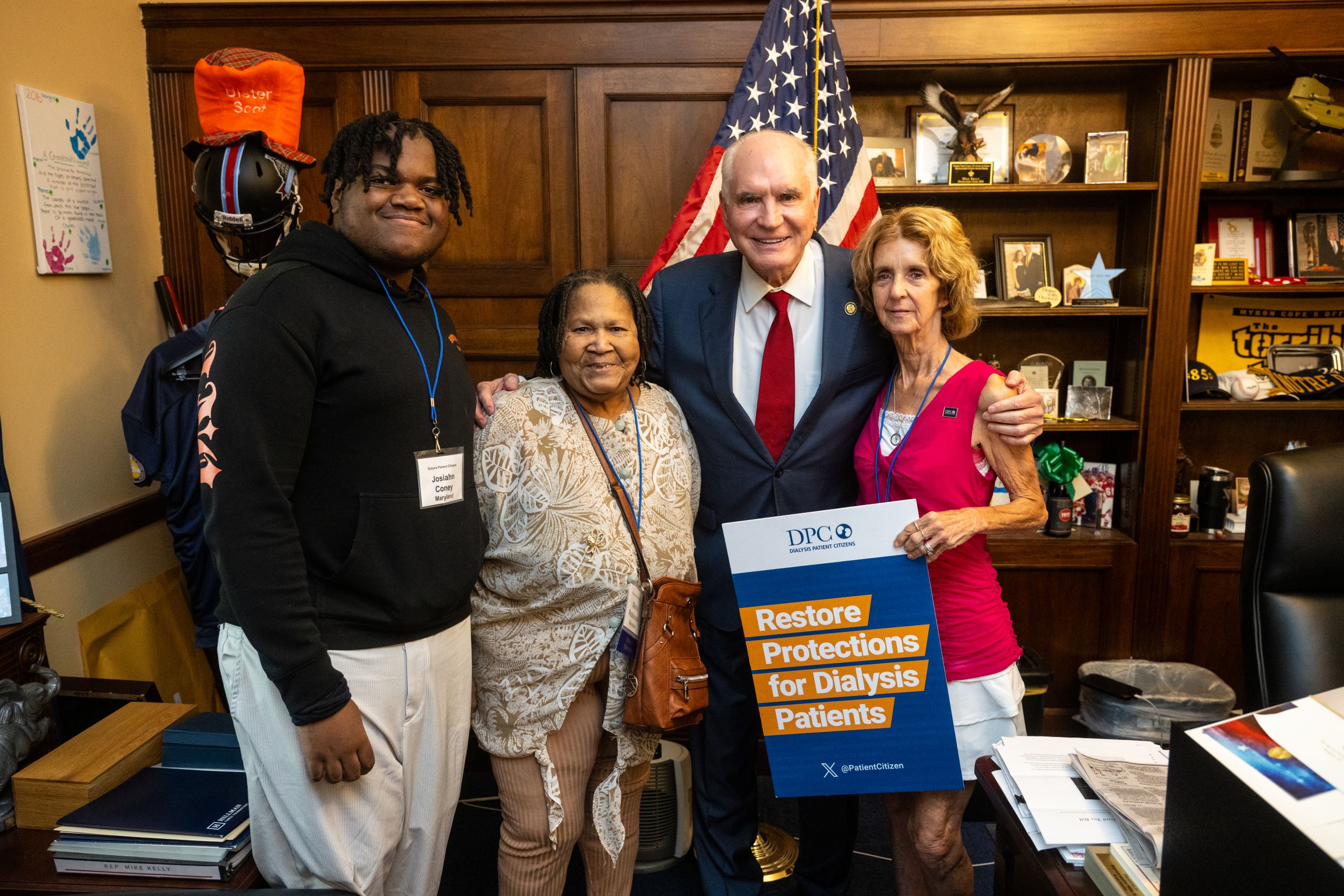
DPC’s 2025 Advocacy Day
Last week, DPC hosted our annual Advocacy Day in Washington, D.C. where we bring together patients, family members, and care givers to meet with their Members of Congress to elevate the patient story for dialysis [...]
Dialysis Patient Citizens Applauds Texas Legislature for Passing Historic Bill Expanding Affordable Medigap Access for Dialysis and ALS Patients
Austin, TX (June 23, 2025) – House Bill 2516 has become public law, a significant victory for Texans living with End-Stage Renal Disease (ESRD), or kidney failure, and Amyotrophic Lateral Sclerosis (ALS). The legislation, [...]
Medigap Protections become Law in Nevada and Texas
Two historic bills that expand affordable access to Medicare Supplement Insurance coverage, otherwise known as Medigap, have passed with overwhelming support in the states of Nevada and Texas this legislative session. Both bills provide affordable [...]
Rhode Island Passes Birthday Rule and Evaluates Community Rating for Medigap Plans
On Friday, June 20, the Rhode Island House passed SB610, Sub B, joining the Senate in approving a birthday rule and evaluation of adopting community rating for all Medicare Supplement plans. SB 610 is awaiting [...]
Delaware Unanimously Passes Medigap Birthday Rule
With a unanimous vote in the Delaware House of Representatives on June 12, the Delaware General Assembly has unanimously passed SB 71 in both chambers. This legislation, called a birthday rule, creates a special open [...]